Abstract
Background: Acute myeloid leukemia (AML) is frequently characterized by mutations in FMS-like tyrosine kinase 3 (FLT3). FLT3 is mutated in one-third of de novo AML patients and recurrent in relapsed/refractory (R/R) AML. More frequent FLT3 internal tandem duplications (ITD) and less frequent tyrosine kinase domain (TKD) point mutations are prognostically important in AML and are associated with an inferior outcome. Although targeted therapy with FLT3 inhibitors improves prognosis in FLT3 mutated AML patients, there is a lack of evidence regarding the superiority of efficacy of various FLT3 inhibitors in clinical practice and the therapeutic pipeline. Broadly grouped as type 1 (targets ITD and TKD, e.g., midostaurin) and type 2 (targets only ITD, e.g., quizartinib) inhibitors, there is no consolidated summary of the difference in efficacy between these two classes of FLT3 inhibitors in R/R AML and high-risk myelodysplastic syndrome (HR-MDS). Hence, we conducted a systematic review and meta-analysis of various type 1 and 2 FLT3 inhibitors tested in clinical trials to compare their clinical effectiveness in treating R/R AML and HR-MDS.
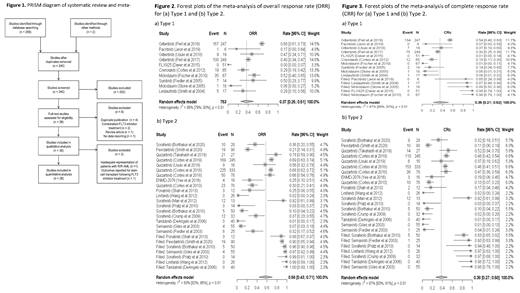
Methods: PubMed and EMBASE databases were searched for clinical trials published between 1/1/2000 and 5/26/2021 using a combination of keywords and subject headings related to FLT3 inhibitors and AML. Two independent reviewers screened titles/abstracts and full texts, with a third reviewer resolving conflicts. Studies were included if they were (1) full-length published journal articles that (2) reported the results of single-arm or double-arm phase I/II/III clinical trials in patients with R/R AML or HR-MDS. Outcomes of interest were composite response rate (CRc=complete response + complete response with incomplete count recovery) and overall response rate (ORR).
Results: Record screening resulted in the initial inclusion of 30 studies for qualitative analysis (Fig. 1). Due to poor representation of R/R AML patients and post-transplant FLT3 inhibitor outcomes, two studies were excluded from quantitative analysis, leaving 28 studies for the final analysis. The studies had a total of 1927 R/R AML and HR-MDS patients with a median age of 61.5 years (range, 13-91) and a median of three (range, 0-10) prior lines of treatment. Giltertinib (n=3 studies) was the most frequently studied type 1 inhibitor, and quizartinib (n=6) and sorafenib (n=5) were the most frequently studied type 2 inhibitors. Heterogeneity testing using Cochran's Q test and I 2 values showed the presence of heterogeneity for both CRc (p<0.01 and I 2=87% for both type 1 and 2) and ORR (p<0.01 for both type 1 and 2, I 2=88% and 92% for type 1 and type 2, respectively) and. Hence, random-effects models were used. Asymmetry tests performed using Egger's linear regression test suggested publication bias only for type 2 (p=0.005) for ORR and type 1 and 2 for CRc (p=0.017 and 0.002, respectively). Thus, the trim-and-fill method was used to adjust for publication bias for type 2 for ORR and type 1 and 2 for CRc. Pooled ORR was 37% (95% CI, 25-51%) for type 1 and 58% (95% CI, 43-71%) for type 2. The highest ORR was for gilteritinib (68%; 95% CI, 61-73%) among type 1 and sorafenib (99%; 95% CI, 81-100%), linifanib (99%; 95% CI, 89-100%), and tandutinib (100%; 95% CI, 93-100%) for type 2 (Fig. 2). Pooled CRc was 35% (95% CI, 21-52%) for type 1 and 38% (95% CI, 27-50%) for type 2. The highest CRc was for midostaurin (98%; 95% CI, 79-100%) among type 1 and sorafenib (97%; 95% CI, 68-100%), tandutinib (98%; 95% CI, 72-100%), and semaxinib (98%; 78-100%) among type 3 (Fig. 3).
Conclusion: Both type 1 and 2 inhibitors are effective as monotherapy in R/R AML and HR-MDS patients. Though not statistically significant, better ORR for type 2 than for type 1 inhibitors in the R/R setting provides a background to explore the biological heterogeneity of response and preferential sensitivity to ITD-targeted therapy alone rather than the dual inhibitor. More prospective randomized study designs comparing type 1 and 2 inhibitors in the R/R and de novo setting are needed.
Maciejewski: Bristol Myers Squibb/Celgene: Consultancy; Regeneron: Consultancy; Alexion: Consultancy; Novartis: Consultancy. Balasubramanian: Servier Pharmaceuticals: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal